“No mother should die bringing life into the world,” declared Karlin Bacher, Director of Clinical Quality Improvement at Jericho Road Community Health Center, during a Delft Imaging webinar. Despite advances in healthcare technology, underserved communities in low- and middle-income countries (LMICs) still face significant challenges. Drawing on his journey from emergency nursing in the U.S. to global health work in Sierra Leone, the Democratic Republic of Congo, and Nepal, Bacher highlighted how solutions like BabyChecker can bridge healthcare gaps and improve maternal health.
A Personal Journey in Global Health
Karlin Bacher began his healthcare career 17 years ago as an ER technician and later as a registered nurse in a busy U.S.-based emergency department. Introducing a portable ultrasound machine in the emergency ward sparked his interest in the technology’s potential. Despite initial scepticism and bureaucratic hurdles, this early experience laid the groundwork for his future endeavours in global health.
Fast forward five years, and Bacher found himself in Sierra Leone, a country with one of the highest maternal mortality rates in the world. “At the time, one in 17 women were expected to die from a maternal health complication,” he recalls.
The Promise and Challenges of Portable Ultrasound
“I’m not really trained in maternal health, but I’m a systems thinker and often found this issue to be overwhelming. During this period of time, I helped host a medical school professor from the Medical College of Georgia. He brought with him an exciting new tool, an ultrasound probe that could be plugged into a small tablet.”
The advent of portable ultrasound devices, which could fit into a small backpack and be powered by a tablet, represented a significant step forward. These devices were not only more affordable but also highly portable, making them ideal for use in remote and resource-poor settings. However, Bacher quickly realized that the training requirements to operate these devices were a major barrier to their widespread adoption.
“We had community health officers who started performing basic obstetric ultrasound scans and became decently skilled at it. But with staffing turnover, we were back at square one,” he explains. This experience highlighted a critical gap: the need for a solution that non-experts could use effectively with minimal training.
This issue of staff turnover and the constant need for retraining is a significant challenge in implementing ultrasound in low-resource settings. When trained personnel leave, the knowledge gap can quickly widen, leaving communities without essential maternal care. It is vital, then, to adopt technologies that reduce the reliance on highly specialised training, enabling even non-experts to perform effective and accurate ultrasound screenings. This not only helps maintain consistent care despite staffing changes but also ensures that essential maternal health services can be delivered more widely and reliably, even in the most resource-constrained environments.

The Leap to AI-Powered Solutions
During an internship with a leprosy-focused global health nonprofit, Bacher’s journey continued as he explored the potential of portable ultrasound in diagnosing subclinical leprosy. The limitation he repeatedly encountered was the human skill factor. This led him to ask a pivotal question: “Could AI solve this problem for us?”
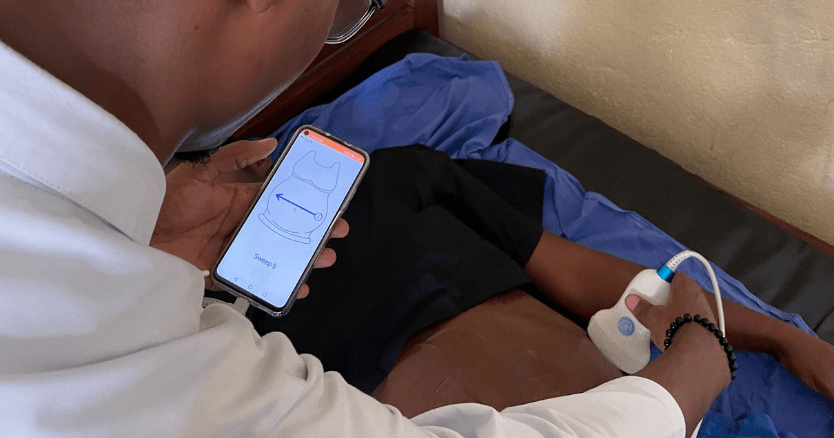
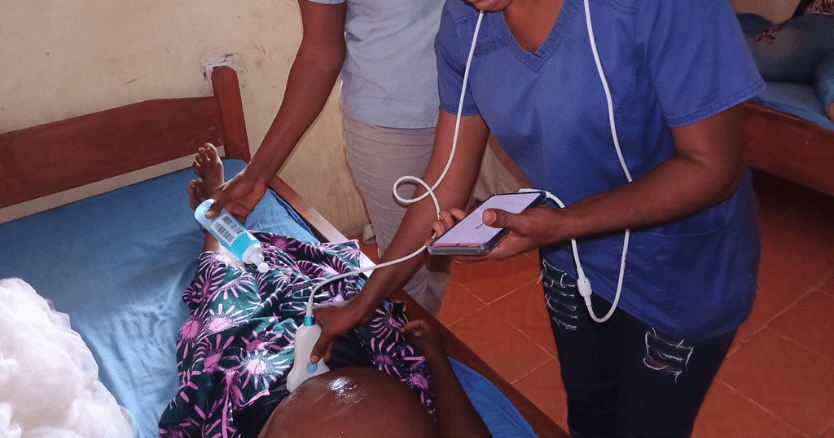
This question set the stage for his encounter with BabyChecker, a smartphone-based Artificial Intelligence (AI) that identifies risks in pregnancy from ultrasound scans. Designed to be portable, affordable, and user-friendly, it can be used by any health worker with no prior expertise in ultrasound. The user is trained through a video to conduct six sweeps across the abdomen, with the BabyChecker application guiding them through the process. Based on these six sweeps, which take one to two minutes to complete, BabyChecker can identify gestational age, foetal presentation, multiple gestations, and placenta localization.
Real-World Impact of BabyChecker
Bacher’s enthusiasm about BabyChecker’s potential led to its deployment in Jericho Road’s clinics in Sierra Leone. The impact was immediate and significant. “Our antenatal attendance rates increased as patients appreciated the reassurance and novelty offered by the scan,” he notes. He shared some compelling stories from the field.
“In August, a woman presented to our regular antenatal clinic for a visit. During the exam, they palpated that the baby’s lie was not cephalic and that her belly was very large. They decided to use the Baby Checker, which estimated 40 to 42 weeks of gestational age. The scan confirmed a breach presentation and a low-lying placenta. It recommended referral to a higher level of care. They carried out this referral, and the lady was sent to the local government hospital. Upon further examination, they identified that the mother was carrying twins. They were able to conduct a c-section successfully. Today, the babies and mother are all doing very well.”
This is not a one-off story. “At the end of September this year, a pregnant mother presented to one of our remote clinics with new-onset vaginal bleeding. Fetal heart rate was still present, so they conducted a BabyChecker scan. The device estimated a gestational age of 35 to 36 weeks and identified a low placenta. The patient was immediately transferred to the government hospital for an emergency C-section. The mother was soon diagnosed with placenta previa. Thanks to early interventions, the mother and child are both alive and doing well today.”
“Fetal heart rate was still present, so they conducted a BabyChecker scan. The device estimated a gestational age of 35 to 36 weeks and identified a low placenta… Thanks to early interventions, the mother and child are both alive and doing well today.”
Challenges and Future Directions
Despite these successes, Bacher acknowledges the challenges that remain. “For widespread adoption, how can we get the word out? How can we make the device radically affordable and ensure an adequate supply chain?” he asks. These questions highlight the need for continued innovation and collaboration to move from pilot projects to widespread use.
Looking ahead, Bacher envisions a broader application of AI-powered diagnostics. “The application of this device to maternal health is promising. But how else can we develop AI algorithms to help community health workers and nurses perform additional diagnostics related to infectious diseases and beyond?” He imagines a future with better diagnostics for conditions like leprosy and tuberculosis.
Conclusion
Karlin Bacher’s journey illustrates the practical potential of technology in global health. From his early experiences in emergency nursing to his work in Sierra Leone, he has seen firsthand how tools like BabyChecker can address gaps in healthcare delivery. However, realizing this potential requires addressing training, affordability, and supply chain challenges.
As we move forward, the lessons from Bacher’s experiences remind us that technology, when thoughtfully integrated and widely accessible, can be a powerful force for improving health outcomes in underserved communities.
You can watch Karlin Bacher’s webinar here:
